How the immune system works
In the world of diseases and parasites, the immune system protects us. It examines everything we eat or touch, catalogs the enemies, and chases them down. But sometimes, it turns against us.
The fact that there’s a special immune system in our bodies that’s responsible for defense against alien bodies, parasites, injuries, and infections, is perhaps common knowledge, yet its workings are quite intricate.
Let’s have a detailed look at how the immune system tests everything we eat and touch, how it chases down enemies, remembers them to not let them harm us again, and how it sometimes turns against us attacking our bodies.
You’ll also learn about the nature of allergies and our bodies’ ability to tolerate some pretty irritant substances.
Immune system and its targets
Our immune system knows how to protect us from the stuff that doesn’t belong to our bodies. It reacts not just to viruses or bacteria but also to the food we eat and the things we touch.
It also prevents the cuts and minor damages from turning into mortal wounds and examines every molecule from out there to know exactly whether it poses a threat.
Generally speaking, the immune system acts against pathogens, that is, against biological things that can cause an illness by consuming our bodies’ resources, emitting toxins, or damaging our tissues.
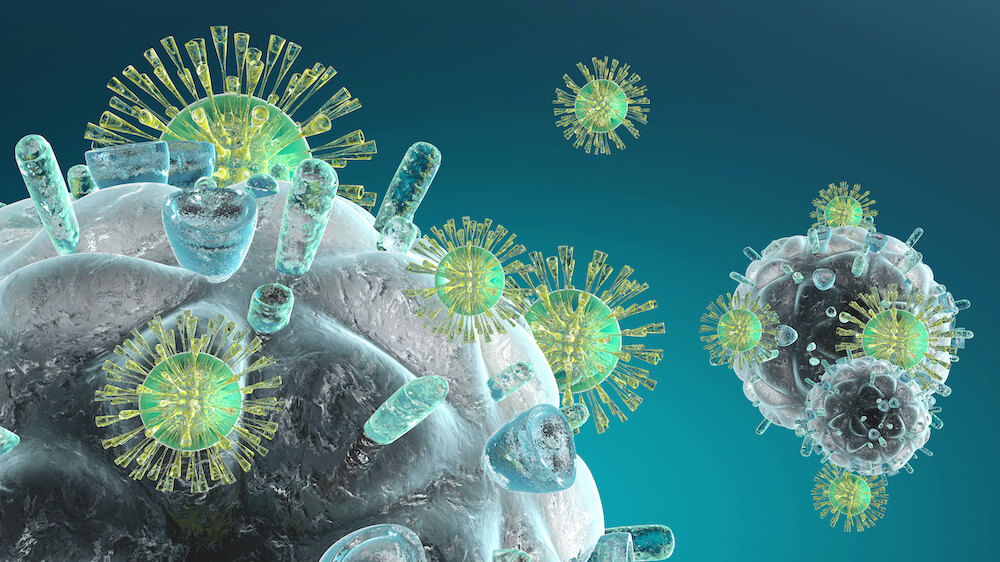
Viruses, bacteria, worms, algae, fungi, and even relatively simple proteins can act as pathogens.

In fact, our immune system reacts to proteins that don’t belong to our bodies. These proteins can be found on the surface of a pathogen or inside it signaling that its genetic code is different from ours.
Our body’s reaction to the same pathogen can vary. Let’s look, for instance, at Streptococcus, a vast genus of bacteria. One of its species, Streptococcus pyogenes, is frequently found on human skin, in throats, and genitals. These bacteria are literally omnipresent which means one might contract it by touching almost anything, anywhere on Earth.
Still, S. pyogenes and its relatives cause severe infections in just about 1% of new cases yearly. Why so?
S. pyogenes bacteria are normally found in our throats. When not kept in check, these bacteria divide more rapidly and become toxic to the host. Most commonly, this results in pharyngitis, also known as strep throat.
In some cases, strep throat causes minor inconveniences and quickly goes away.
Sometimes it returns shortly after having been cured—that is, becomes recurrent or chronic.
Sometimes, S. pyogenes cause additional problems like rheumatic heart disease.
Are there reasons for these differences in damage?
Research of the 2000s-2010s suggests that some patients with recurrent strep throat, especially young children, might be genetically prone to it, while in some patients S. pyogenes seems to simply seize the day (because of the host’s malnutrition, for example). This means our bodies can apply different immunity strategies to certain pathogens, and sometimes these strategies can fail.
Let’s see which strategies our immune system applies to keep us safe from such infections as Streptococcus, and how they work.
Basically, there are two of them, and two types of immune systems implement them, respectively: innate and adaptive.
Allies and agents of the innate immune system
As you already know, there are two types of immune systems. The Innate immune system works non-specifically and applies one mechanism to all pathogens.

Many organisms including plants, fungi, primitive multicellular organisms, and insects have developed their versions of innate immunity.
The innate immune system works as the first line of defense, for instance, employing anatomical barriers that prevent pathogens from getting inside.
What are these barriers?
Tears, sweat, saliva, enzymes, mucus in the gut and lungs—all these contain proteins that can damage pathogens arriving on our threshold.
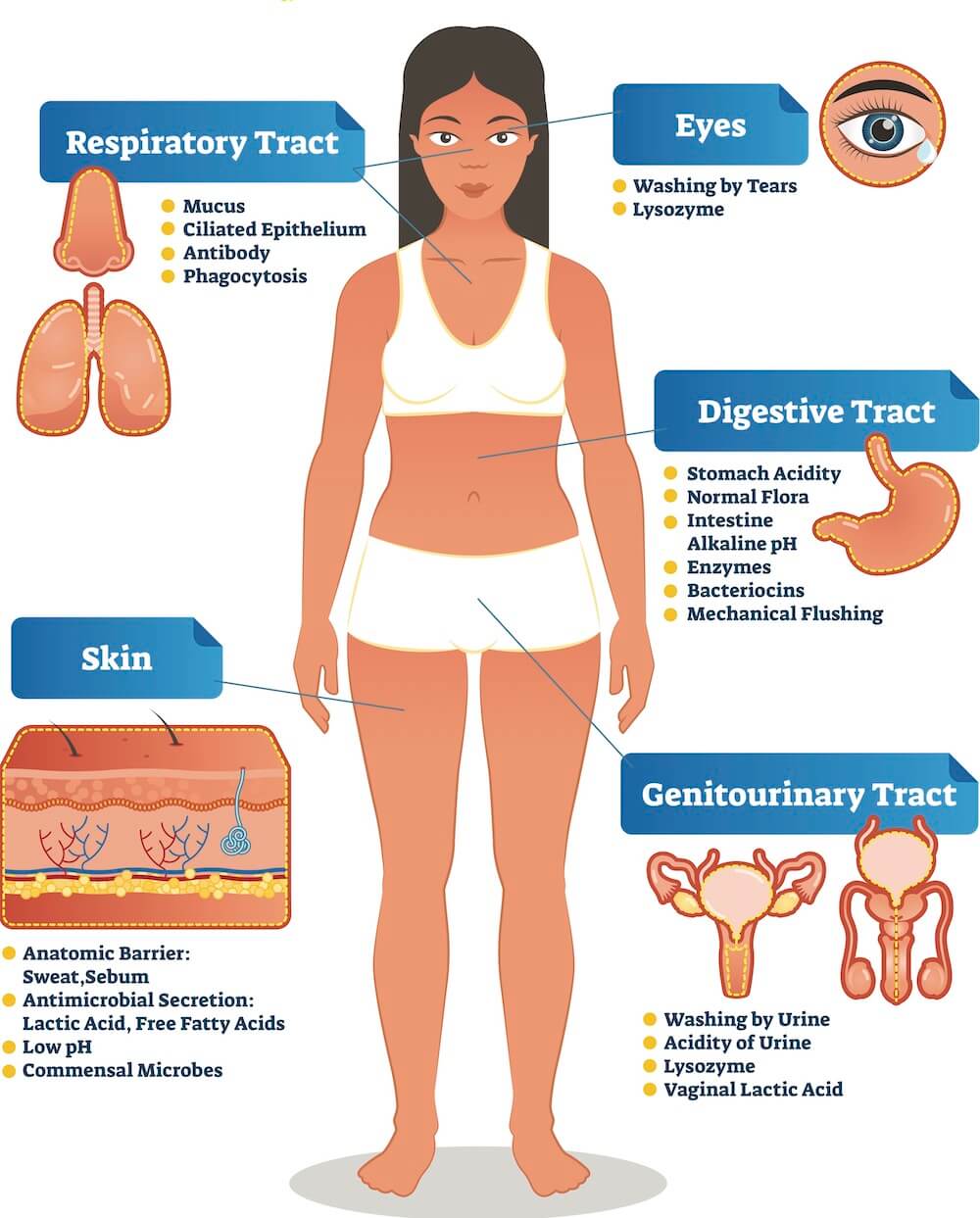
For example, lysozyme in saliva, tears, and mucus damages the outer membranes of bacterial cells and thus protects us against microscopic threats hidden in the food we eat and surfaces we touch. It’s lysozyme that kills such common bacteria as Streptococcus.
Here’s what a molecule of lysozyme looks like:

Lysozyme is also found in breast milk. It helps to protect an infant from infections and populate its intestine with friendly microorganisms (microflora) by keeping harmful ones at bay.

Our microflora, in its turn, also does a great deal acting in alliance with our innate immune system.
Gut bacteria create stable colonies on the inner surface of our guts and prevent unfamiliar bacteria from reproducing. Gut bacteria also secrete toxic compounds damaging harmful bacteria.
Let’s see what the immune system does to spot intruders.
How does the immune system know its enemies?
Every tissue in our bodies has detectors sensitive to pathogens. These detectors are pattern recognition receptors (PRR) and toll-like receptors (TLR).
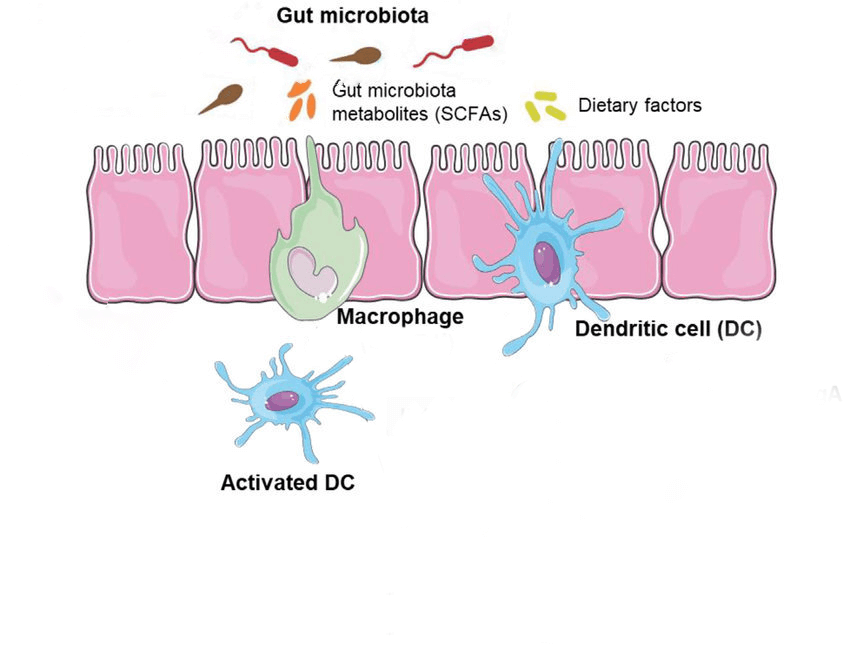
These receptors are located on the surfaces of immune cells like macrophages, monocytes, neutrophils, dendritic cells, and even epithelial cells.

Cells like macrophages and neutrophils know how to cope with pathogens after detecting them with PRRs. How?
Many common pathogens have typical surface structures easily recognized by the PRRs or TLRs. They are called pathogen-associated molecular patterns (PAMPs) that can be found on many common infectious agents.
We inherit genes for pattern recognition and toll-like receptors which means evolution has already taken care of us and left instructions on how to cope with pathogens our ancestors had already met.
Pattern-recognition receptors are found in most tissues inside our bodies—even in dental pulp, protecting teeth from diseases.
These receptors are also common inside our guts: tissues of the intestinal tract include immune cells containing PRRs.
PRRs are sensitive not only to pathogen receptors but also to our own cells that have been damaged and must be destroyed. PRRs recognize these cells with the help of damage-associated molecular patterns (DAMP). These patterns are molecules released by damaged cells. They signal for launching cell suicide—apoptosis—and defend surrounding tissues from toxins.
DAMPs are also released by infected cells that must be destroyed by the immune system to stop pathogens from spreading.
It’s interesting that an excessive number of PAMPs and DAMPs, that is patterns of damage and pathogen presence, is associated with ageing and cancer.
PAMPs and DAMPs take part in inflammation processes that damage cells. Accumulation of such damages is one of the reasons for cancer and ageing. Course block
As you can see, receptors in immune cells are crucial for recognizing pathogens and damages.
Unfortunately, sometimes the very same receptors allow pathogens in.
For example, human white blood cells have receptors on their surfaces to which HIV can bind. People who carry a mutation for this receptor are resistant to HIV because viruses can’t bind to their immune cells.
But what happens after pathogens meet immune cell receptors?