When Mold Became Medicine: The History of Antibiotics

Bacterial pneumonia, tuberculosis, syphilis, plague, and wound infections are just a few of the bacterial diseases that were life-threatening and had high mortality rates before antibiotics were discovered. Antibiotics are essential medicines that have revolutionized healthcare by effectively treating bacterial infections. This article will explore the history of antibiotics, how they function, and the challenges posed by antibiotic resistance.
What are antibiotics, and how do they work?
The word “antibiotic” is derived from ancient Greek: anti, meaning “against,” bios,” meaning “life.” Initially, the term was a general concept used for anything harmful to living organisms.
Nowadays, the term is applied to medicines used to treat infections caused by bacteria. Antibiotics fight bacterial infections in two main ways: by killing the bacteria or by stopping their growth.

In the first case, antibiotics target essential parts of the bacterial cell, like the wall or membrane. The cell wall is crucial for the bacteria’s survival because it maintains the cell’s shape and prevents it from bursting. When the cell wall is damaged, the bacteria can’t survive. Other antibiotics damage the bacterial cell membrane, causing the cell’s contents to leak, leading to the bacteria’s death.
In the second case, antibiotics prevent bacteria from growing (they are called bacteriostatic). These antibiotics interfere with the bacteria’s ability to produce proteins or its DNA replication process. Without proteins and DNA replication, the bacteria can’t multiply.

One of the key principles of antibiotics is selective toxicity. This means the antibiotics are designed to target only bacterial cells without harming humans. This is possible because bacterial cells are different from human cells in several ways, such as the structure of their walls and the way they produce proteins. Then again, there are different types of antibiotics here: broad and narrow spectrum. The first targets a wide range of bacteria, both good and bad. They are helpful when the exact cause of an infection is unknown. Still, they can also disrupt the beneficial bacteria in the body, leading to side effects like diarrhea or yeast infections. The narrow-spectrum antibiotics target specific types of bacteria. They are used when the exact cause of an infection is known, minimizing damage to beneficial bacteria and reducing the risk of side effects.
Discovery of antibiotics
Since ancient times, various cultures used natural remedies, including molds, to treat infections and diseases. These ancient practices were based on observations that certain natural substances improved healing and prevented infections. While people didn’t understand bacteria or molds scientifically, they relied on trial and error and passed down effective treatments through generations.

For example, the ancient Egyptians applied moldy bread to wounds to prevent infections. Greek and Roman physicians like Hippocrates and Galen used moldy bread and wine-soaked cloths to clean wounds. They believed these substances could prevent infections. In ancient China, moldy soybean curd (tofu) was used to treat skin infections as early as 3000 BC.

During the Middle Ages, people noticed that wounds treated with moldy cheese healed better than those left untreated.

Modern antibiotics were discovered by accident in 1928 by Alexander Fleming, a Scottish bacteriologist. He conducted experiments with Staphylococcus bacteria in a lab at St. Mary’s Hospital in London. He went on vacation, leaving behind some petri dishes. Returning, he noticed that a mold called Penicillium notatum had contaminated one of his petri dishes containing bacteria. Surprisingly, the bacteria surrounding the mold had been destroyed while areas farther away continued to thrive.

Fleming extracted a substance and conducted experiments that showed its effectiveness against harmful bacteria, including Staphylococcus, Streptococcus, and other pathogens. He named this substance “penicillin.”

Fleming faced many challenges in further developing penicillin for widespread use. Its initial forms were unstable and contained impurities, and it was challenging to create a purification process and scale up penicillin production at the time.
In the 1940s, a team of Oxford University researchers led by Howard Florey and Ernst Chain refined the production methods that enabled the mass production of penicillin. Their contribution was highly important during the break of World War 2, as there was a need for effective treatments for wounded soldiers. By the mid-1940s, penicillin was widely used to treat infections in soldiers and civilians.

In 1945, Alexander Fleming, Howard Florey, and Ernst Boris Chain received the Nobel Prize in Medicine for their work on penicillin.
The mass production and use of penicillin during World War II marked a turning point in medicine. It saved countless lives and drastically reduced the mortality rate from bacterial infections.
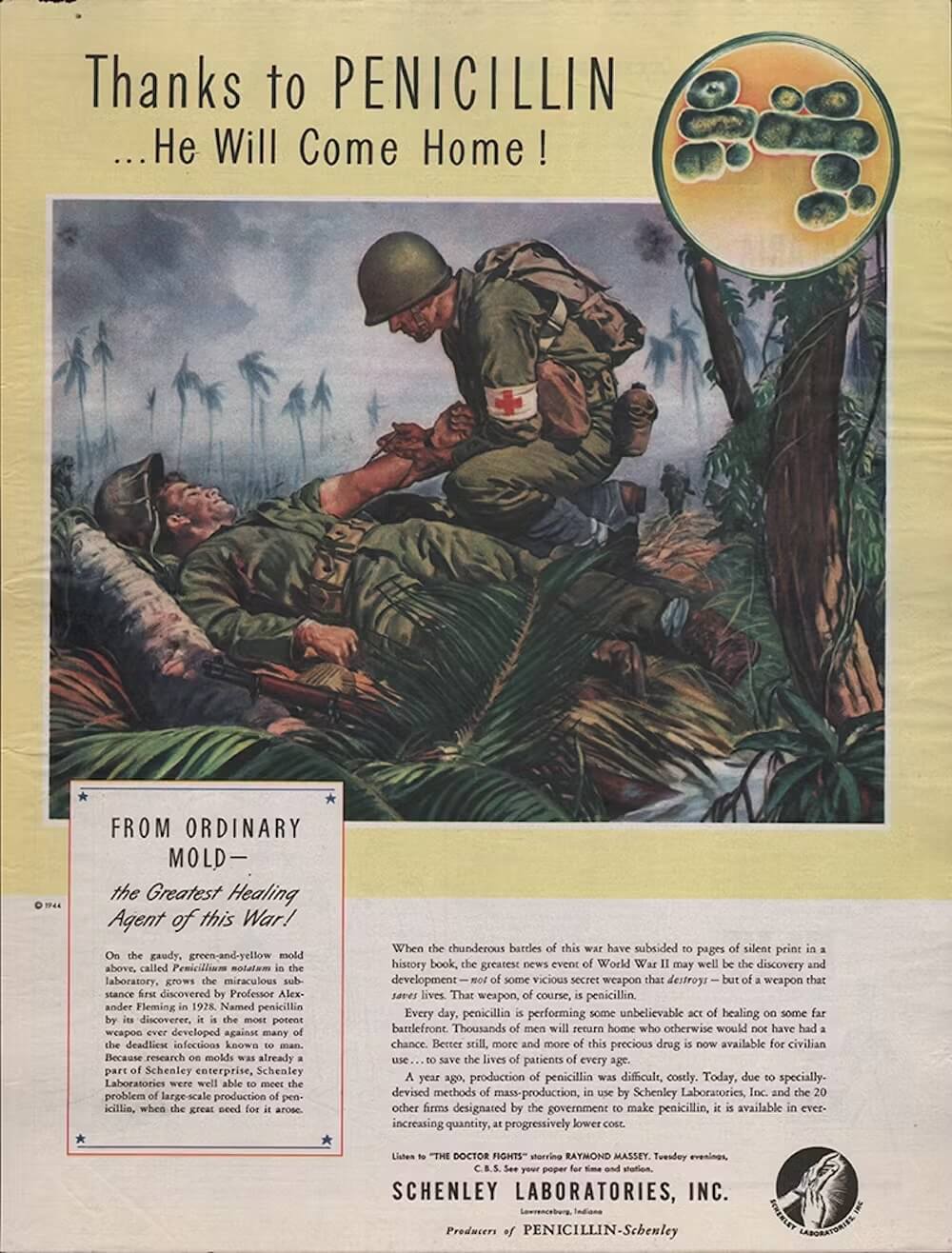
Penicillin was revolutionary because it was the first substance found to effectively kill bacteria without harming human cells. It was the first time doctors had a powerful tool to treat bacterial infections, which were often deadly.

Flaming’s discovery of antibiotics was accidental, but one predecessor of penicillin is often considered the first antibiotic. In 1909, the German scientist Paul Ehrlich searched for a compound to treat Syphilis. This sexually transmitted infection caused by the bacterium Treponema pallidum was a major health problem at the time. Ehrlich and his colleague Sahachiro Hata developed Salvarsan, the first drug to cure this infection effectively.

Salvarsan was a man-made chemical compound that included arsenic. Consequently, the drug had to be administered carefully and had significant side effects, which limited its broader use.

However, Salvarsan marked the beginning of the chemotherapy era in medicine, where specific drugs were developed to target specific diseases.

So, why do we usually name penicillin the first antibiotic?
The reason lies in the definition. The term “antibiotic ” refers to substances produced by microorganisms that can kill or inhibit the growth of other microorganisms. Penicillin is considered the first true antibiotic because it is a natural substance produced by a mold (a living organism) that influences other microorganisms.
Plus, unlike Salvarsan, penicillin could treat many bacterial infections, including pneumonia, strep throat, and wound infections, making it much more versatile.
Finally, Penicillin had fewer and less severe side effects than Salvarsan, making it safer for widespread use.
What are some other significant antibiotics?
After the discovery of penicillin, several other important antibiotics were discovered that have played a crucial role in treating bacterial infections.
Streptomycin
In 1943, Selman Waksman, Albert Schatz, and Elizabeth Bugie discovered streptomycin in the USA. Streptomycin was the first antibiotic effective against tuberculosis (TB). It was derived from a soil bacterium called Streptomyces griseus. Streptomycin was a game-changer in treating TB and was used as a monotherapy, meaning it was the only drug given to patients with TB. In 1952, Waksman received the Nobel Prize for Physiology and Medicine for discovering streptomycin.

Within the first few years of streptomycin usage, bacteria causing TB began to resist it. This was a significant problem because tuberculosis could no longer be effectively treated with streptomycin alone. So, scientists introduced combination therapy, where patients were treated with multiple drugs. This approach made it much harder for the bacteria to become resistant because they would need to develop resistance to several different antibiotics simultaneously.
Streptomycin is still used today but is not the first choice for treating TB. Nonetheless, the antibiotic still effectively treats other bacterial infections, like plague and tularemia.
Tetracycline
In 1948, Benjamin Minge Duggar, an American biochemist, discovered tetracycline while working for Lederle Laboratories in the USA. Tetracycline is a broad-spectrum antibiotic, incredibly useful for treating many infections, from severe acne to pneumonia and bronchitis.
Tetracycline interferes with bacteria’s ability to produce proteins essential for their growth and survival. Without these proteins, the bacteria cannot multiply and spread, allowing the body’s immune system to fight off the infection more effectively. That said, over time, some bacteria have developed resistance to tetracycline, meaning it no longer works as well against them.
What is antibiotic resistance, why does it occur, and what does it mean for our health?
Initially, antibiotics were seen as miracle drugs. They were highly effective in treating bacterial infections and saved millions of lives. However, the overuse and misuse of antibiotics have led to a significant problem: antibiotic resistance. This means some bacteria have evolved to withstand the drugs that once killed them, creating what we now call “superbugs.”
Resistance starts with the mutation of harmful bacteria. During the process of bacteria reproduction, mutations (random changes in their DNA) can happen. Some mutations may help bacteria survive an antibiotic attack.
Moreover, bacteria can share genes with each other, even across different species. If one bacterium has a resistance gene, it can pass it to others, spreading the ability to resist certain drugs.
When antibiotics kill off susceptible bacteria, resistant ones survive and multiply. This process resembles natural selection, where only the fittest organisms survive.

Scientists are exploring new ways to create antibiotics that can overcome resistance. This includes developing drugs that target different parts of bacterial cells or that work in novel ways. However, the development of new antibiotics has slowed down.
Nowadays, scientists are exploring new and innovative ways to treat bacterial infections.
For example, there is phage therapy, which uses bacteriophages, special viruses that specifically target and kill bacteria. Each type of phage targets certain bacteria. When a phage finds its target bacteria, it attaches to it and injects its genetic material. The phage then takes over the bacterial cell’s machinery to reproduce itself, eventually causing the bacteria to burst open and die, releasing new phages that can infect more bacteria. The challenge with phage therapy is that it needs to be created for the specific type of bacteria, which can be time-consuming.
The future of antibiotics depends on our ability to adapt and innovate. By developing new antibiotics, exploring alternative treatments, improving diagnostic tools, promoting responsible use, and educating the public, we can extend the effectiveness of antibiotics for many years to come.